Cancer Screening in Schizophrenia:
All Hands on Deck

Source: https://www.firstquotehealth.com/health-insurance-news/the-fight-against-breast-cancer
Should the quality of one’s cancer care be worse if a person is diagnosed with schizophrenia (or any mental health condition for that matter) compared to people who are not diagnosed with this mental illness? Of course, it should not. This month I came across an article on rates of breast cancer screening in women with schizophrenia (1). In this meta-analysis (this is a way of combining studies to look at large samples) that included over 25,000 women with schizophrenia, the authors found that women with schizophrenia were half as likely as the general population to receive recommended breast cancer screening (i.e., having a mammogram). This is unfortunately another example of substandard medical care received by individuals with schizophrenia.
“…women with schizophrenia are half as likely as the general population to receive recommended breast cancer screening…”
The importance of this publication hit home for me as it aligns with my clinical experience. I have been working in a community mental health center for the past 20 years. Over the last decade, as I have gotten older alongside my patients, I have lost many patients due to heart disease and, increasingly, cancer. In one French study, cancer was the second leading cause of death for individuals with schizophrenia, after suicide (2). In psychiatry, we have always paid attention to suicide. In the last decade, our attention also focused on heart disease; we need to tackle cancer next.
Screening is but one aspect of optimal cancer care. For those with schizophrenia and breast cancer, care can break down at many levels: they get diagnosed later, when cancer is harder to treat; they get substandard treatments; and they get incomplete follow-up. As a result, they die earlier compared to their peers without a psychiatric diagnosis (3). If we want to begin to correct this unfair health inequality, care providers must adopt an all hands on deck attitude. Psychiatry must engage patients around cancer prevention and care in all settings: doctor’s offices (both primary care and medical specialties), mental health centers, communities, and at home.
“…to correct this unfair health inequality, care providers must adopt an all hands on deck attitude…”
Group homes, outreach workers and families need to be educated about the importance of preventive care, such as breast cancer screening. For example, many patients and families may not be aware of the high importance of catching breast cancer early—close to 100% of breast cancer is curable if detected before it grows and spreads:
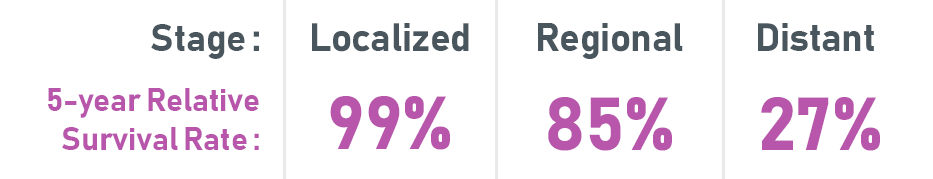
5-year Relative Survival Rates for Breast Cancer (2019.) Retrieved from the American Cancer Society: https://www.cancer.org/cancer/breast-cancer/understanding-a-breast-cancer-diagnosis/breast-cancer-survival-rates.html
Psychiatric clinics must work towards better communication and care coordination between psychiatry and medicine. In our clinic, we began an initiative CHAMPS (Coordinated Health And Medical Prevention Service) that includes metabolic monitoring (i.e., blood tests to measure diabetes and heart disease risk) to which we are now adding the tracking of recommended prevention measures such as cancer screening. A colleague of mine at Massachusetts General Hospital, Dr. Kelly Irwin, has created the Engage Initiative, a program that connects patients with serious mental illness (SMI) to high-quality and state-of-the-art academic cancer care (4). Click here to visit the Engage Initiative website.
A final word to my fellow psychiatrists and colleagues who may be nervous about a broadening of their job description: I am not advocating that psychiatrists suddenly begin cancer screening at the expense of core psychiatric tasks. However, knowledge of cancer screening guidelines (e.g., those from the US Preventive Services Task Force (5)), making cancer screening part of clinical conversations, connecting a patient to primary care, and supporting ambivalent patients in making a mammography visit are reasonable expectations that should not be controversial. Staying on the sidelines and ignoring the medical health of people with SMI should be.
The United States Preventive Services Task Force recommends that women who are 50 to 74 years old and are at average risk for breast cancer get a mammogram every two years. For some women, starting routine screening for breast cancer earlier, at age 40 and more often, once a year may make sense. Every woman should discuss the best screening schedule for her situation with her doctor.
Oliver Freudenreich, MD, FACLP
Co-Director, MGH Schizophrenia Clinical and Research Program
References
Hwong A, Wang K, Bent S, Mangurian C. Breast cancer screening in women with schizophrenia: a systematic review and meta-analysis. Psychiatr Serv. 2019:appips201900318.
Tran E, Rouillon F, Loze JY, Casadebaig F, Philippe A, Vitry F, et al. Cancer mortality in patients with schizophrenia: an 11-year prospective cohort study. Cancer. 2009;115(15):3555-3562.
Dalton SO, Suppli NP, Ewertz M, Kroman N, Grassi L, Johansen C. Impact of schizophrenia and related disorders on mortality from breast cancer: A population-based cohort study in Denmark, 1995-2011. Breast. 2018;40:170-176.
Irwin KE, Freudenreich O, Peppercorn J, Taghian AG, Freer PE, Gudewicz TM. Case records of the Massachusetts General Hospital. Case 30-2016. A 63-Year-old woman with bipolar disorder, cancer, and worsening depression. N Engl J Med. 2016;375(13):1270-1281.
US Preventive Services Task Force. Available from: https://www.uspreventiveservicestaskforce.org/Page/Name/home.